Breast cancer is a topic close to the hearts of many, as it affects countless individuals around the world. This formidable disease strikes both women and men, causing concern and raising awareness about its devastating impact. In this section, we will provide you with a heartfelt introduction to breast cancer, offering key details that will help you understand its significance.
Breast cancer, simply put, is a type of cancer that originates in the breast tissue. The cells within the breast undergo abnormal growth and division, leading to the formation of tumors. These tumors can infiltrate nearby tissues and, if left unchecked, spread to other parts of the body.
It is important to know that breast cancer comes in various forms, each with its unique characteristics. The most common types include ductal carcinoma, originating in the milk ducts, and lobular carcinoma, which begins in the milk-producing lobules. Other types, such as inflammatory breast cancer and Paget’s disease, although less common, require our attention due to their distinct traits.
Breast cancer is not a matter to be taken lightly, as its prevalence is significant. Across the globe, it stands as the most commonly diagnosed cancer among women. The impact is felt in both developed and developing countries, transcending borders and affecting lives. While women are primarily affected, it is essential to acknowledge that breast cancer can also strike men, albeit at a lower rate.
Understanding breast cancer involves exploring the risk factors that contribute to its development. While there is no single cause, certain factors can increase an individual’s susceptibility. Age and gender play a role, with the risk rising as one grows older. Genetic and family history can also heighten the chances of developing breast cancer. Hormonal factors, lifestyle choices, and environmental influences all contribute to this complex equation.
By delving into the details of breast cancer, we gain a deeper understanding of its impact and the importance of early detection. In the following sections of this comprehensive guide, we will explore the symptoms, screening methods, treatment options, and preventive measures associated with breast cancer. Empower yourself with knowledge as we navigate this journey together, supporting one another in the fight against breast cancer.
Types of Breast Cancer

When it comes to breast cancer, it’s crucial to understand that it encompasses various types, each with its own characteristics and implications. By familiarizing ourselves with the different types of breast cancer, we can better comprehend the complexity of this disease and the diverse approaches to its diagnosis and treatment. Let’s explore these types in more detail:
- Ductal Carcinoma: Ductal carcinoma is the most common type of breast cancer, accounting for approximately 80% of cases. It originates in the cells lining the milk ducts, which are responsible for carrying milk from the lobules to the nipple during breastfeeding. Ductal carcinoma can present as invasive (spreading beyond the ducts) or in situ (confined to the ducts).
- Lobular Carcinoma: Lobular carcinoma begins in the milk-producing glands, called lobules, and accounts for around 10-15% of breast cancer cases. Unlike ductal carcinoma, which typically forms a lump, lobular carcinoma may be less defined and spread out, making it harder to detect through imaging. Lobular carcinoma can also be invasive or in situ.
- Inflammatory Breast Cancer: Inflammatory breast cancer is a rare and aggressive form of breast cancer. It accounts for a small percentage of cases but requires immediate attention due to its rapid growth and distinctive characteristics. It often manifests as redness, swelling, warmth, and a pitted appearance of the breast skin. Inflammatory breast cancer can progress quickly and may not present as a distinct lump, making diagnosis challenging.
- Paget’s Disease of the Breast: Paget’s disease of the breast is a rare form of breast cancer that typically starts in the milk ducts and spreads to the nipple and areola. It often manifests as flaky, crusty, or itchy skin around the nipple, resembling eczema. Although it is usually associated with underlying ductal carcinoma, it can occur without an evident lump.
- Triple-Negative Breast Cancer: Triple-negative breast cancer refers to a subtype of breast cancer where the cancer cells lack receptors for estrogen, progesterone, and HER2 protein. This type of breast cancer tends to be more aggressive and challenging to treat, as it does not respond to hormonal therapies or targeted treatments specific to HER2.
Understanding the various types of breast cancer allows healthcare professionals to tailor treatment plans to each patient’s specific needs. It highlights the importance of accurate diagnosis through biopsy and imaging techniques, which provide insights into the tumor’s characteristics and behavior. By staying informed about the distinct types of breast cancer, we can further support ongoing research and advancements in treatment options, leading us closer to improved outcomes for those affected by this disease.
Risk Factors for Breast Cancer
Breast cancer can affect anyone, but certain factors can increase an individual’s likelihood of developing the disease. By understanding these risk factors, we can take proactive steps towards prevention, early detection, and effective management. Here are some key risk factors associated with breast cancer:
- Age and Gender: Age plays a significant role in breast cancer risk. The risk increases as individuals grow older, with most breast cancers being diagnosed in women over the age of 50. However, it’s important to note that breast cancer can occur at any age, including in younger women and even in men, although it is less common.
- Genetic and Family History: Inherited gene mutations can significantly impact breast cancer risk. The most well-known gene mutations associated with breast cancer are BRCA1 and BRCA2. Individuals with a family history of breast or ovarian cancer, especially in first-degree relatives (parents, siblings, children), may have a higher risk of developing breast cancer.
- Hormonal Factors: Hormonal factors play a crucial role in breast cancer development. Women with prolonged exposure to estrogen due to early onset of menstruation (before age 12), late menopause (after age 55), or starting hormone replacement therapy at an early age may have an increased risk. Additionally, women who have never been pregnant or had their first pregnancy after the age of 30 are at higher risk.
- Lifestyle Factors: Certain lifestyle choices can influence breast cancer risk. Factors such as excessive alcohol consumption, smoking, lack of physical activity, and obesity have been associated with an increased likelihood of developing breast cancer. Adopting a healthy lifestyle that includes regular exercise, a balanced diet, limited alcohol intake, and avoiding smoking can help reduce the risk.
- Environmental Factors: While the exact impact of environmental factors on breast cancer is still being studied, exposure to certain substances and environmental pollutants may contribute to an increased risk. Prolonged exposure to ionizing radiation, such as during medical imaging tests, and certain workplace chemicals like benzene and certain pesticides have been linked to an elevated risk of breast cancer.
It’s important to note that having one or more of these risk factors does not guarantee the development of breast cancer. Many individuals without any known risk factors can still develop breast cancer, while others with multiple risk factors may never be affected. Risk factors provide valuable information to healthcare professionals, allowing for personalized risk assessments and targeted interventions.
By being aware of these risk factors, individuals can make informed decisions about their health and take proactive steps toward breast cancer prevention. Regular breast self-examinations, clinical breast examinations, and mammograms are essential tools for early detection. Additionally, maintaining a healthy lifestyle, staying physically active, and avoiding exposure to harmful substances can contribute to reducing the risk of breast cancer and promoting overall well-being.
Symptoms of Breast Cancer
Recognizing the symptoms of breast cancer is crucial for early detection and prompt medical intervention. While some cases of breast cancer may not exhibit noticeable symptoms in the early stages, it’s essential to be vigilant and aware of any changes in your breasts. Here are some common symptoms that may indicate the presence of breast cancer:
- Breast Lump or Thickening: The most common symptom of breast cancer is the presence of a new lump or mass in the breast or underarm area. This lump may feel different from the surrounding breast tissue and can vary in size. However, it’s important to note that not all breast lumps are cancerous, as some may be benign cysts or fibroadenomas. Nevertheless, any new lump or thickening should be evaluated by a healthcare professional.
- Changes in Breast Size or Shape: Breast cancer may cause noticeable changes in the size or shape of the breast. This could manifest as swelling, shrinkage, or asymmetry between the breasts. It’s important to be aware of any unexplained changes in breast appearance that persist over time.
- Breast Pain or Discomfort: While breast pain is a common symptom experienced by many individuals, it is not typically associated with breast cancer. However, persistent or localized pain in the breast or nipple that doesn’t seem to be related to the menstrual cycle or any specific injury should be evaluated by a healthcare professional.
- Changes in Breast Skin: Breast cancer may cause changes in the skin texture or appearance of the breast. These changes can include redness, dimpling, puckering, or the skin appearing like an orange peel (peau d’orange). Additionally, any rash, eczema-like symptoms, or persistent itching on the breast or nipple should be assessed by a medical professional.
- Nipple Changes: Changes in the nipple can be indicative of breast cancer. Look out for nipple inversion (when the nipple turns inward), nipple discharge (other than breast milk), or any changes in the nipple’s shape, color, or texture.
- Swollen Lymph Nodes: Breast cancer may cause the lymph nodes under the arm or around the collarbone to swell or feel tender. However, it’s important to note that swollen lymph nodes can also be a result of infection or other non-cancerous conditions.
It’s important to remember that these symptoms are not exclusive to breast cancer and can have various causes. However, if you notice any persistent changes or abnormalities in your breasts that concern you, it is recommended to consult with a healthcare professional for further evaluation. Regular self-examinations, in addition to routine clinical breast examinations and mammograms as per recommended guidelines, play a crucial role in detecting breast cancer at its early stages when treatment options and outcomes are generally more favorable.
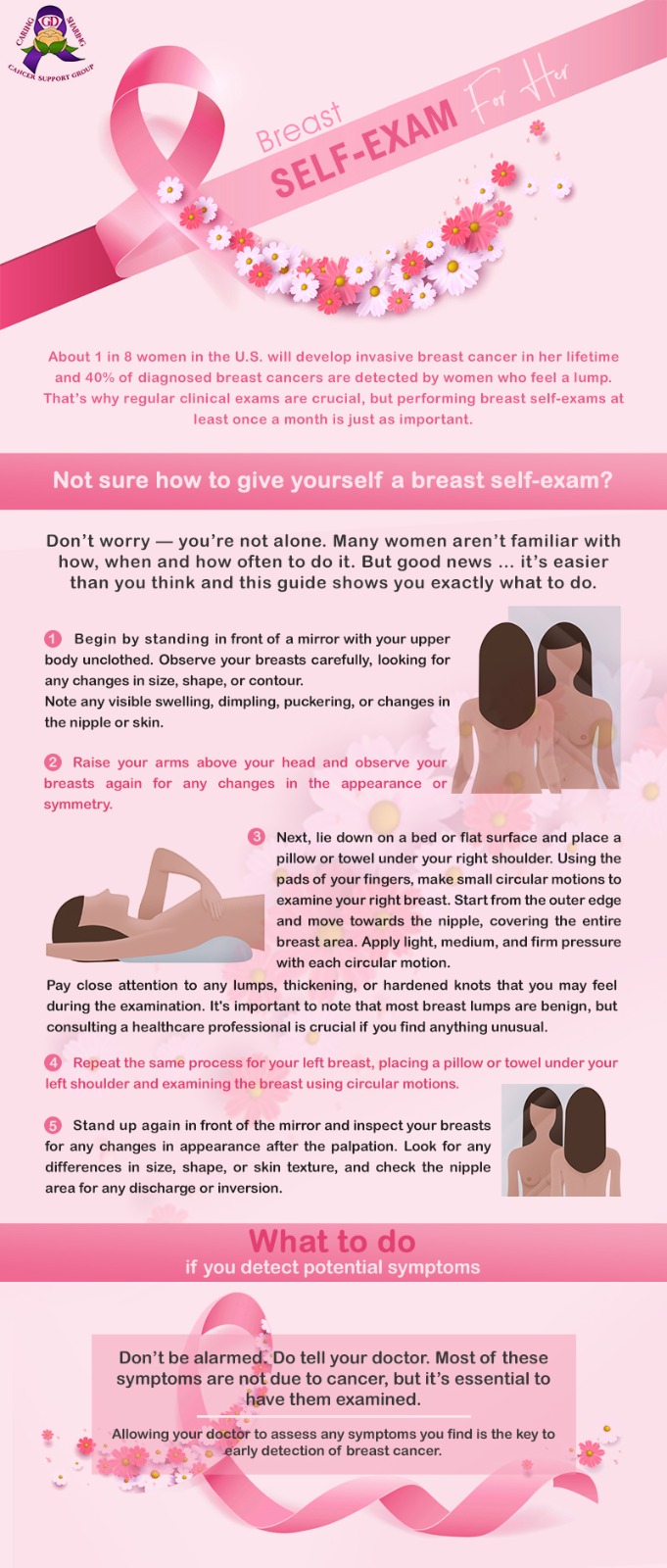
How to Do Breast Self-Exam?
Breast Cancer Screening and Diagnosis
Screening and early detection are vital in the fight against breast cancer, as they can lead to earlier diagnosis and improved treatment outcomes. Regular screenings and prompt follow-up on any suspicious findings are key to detecting breast cancer at its earliest stages. Here’s an overview of breast cancer screening and diagnosis methods:
Mammography
Mammography is the most common screening tool for breast cancer. It involves taking X-ray images of the breast to detect any abnormal masses or calcifications that may indicate cancer. Mammograms are recommended for women starting at the age of 40, although guidelines may vary depending on factors such as family history and individual risk. Regular mammograms every one to two years can help detect breast cancer in its early stages, even before symptoms become noticeable.
Clinical Breast Examination (CBE)
A clinical breast examination is a physical examination of the breasts performed by a healthcare professional. During a CBE, the doctor or nurse will carefully feel the breasts and underarm areas for any lumps or abnormalities. CBEs are often performed in conjunction with mammograms and can provide additional information about breast tissue.
Breast Self-Examination (BSE)
Breast self-examination involves regularly checking your own breasts for any changes or abnormalities. While BSE is no longer recommended as a stand-alone method for breast cancer screening, it is still valuable for women to become familiar with their breasts and report any changes to their healthcare provider.
Imaging Techniques
In addition to mammography, other imaging techniques may be used to further evaluate suspicious findings or assist in the diagnosis of breast cancer. These include:
Ultrasound: Ultrasound uses sound waves to create images of the breast tissue. It can help determine whether a lump is solid or filled with fluid (cystic) and can be used to guide needle biopsies if needed.
Magnetic Resonance Imaging (MRI): MRI uses powerful magnets and radio waves to create detailed images of the breast. It is often used in specific cases, such as for individuals at high risk or to provide additional information when other imaging tests are inconclusive.
Biopsy
A biopsy is the definitive diagnostic procedure for breast cancer. It involves the removal of a small tissue sample from the suspicious area in the breast for laboratory analysis. The biopsy can be done using various techniques, including needle biopsy (fine-needle aspiration, core needle biopsy) or surgical biopsy (excisional biopsy or incisional biopsy). The analysis of the biopsy sample determines whether cancer cells are present and helps determine the type and characteristics of breast cancer.
Genetic Testing
Genetic testing may be recommended for individuals with a strong family history of breast cancer or those who meet certain criteria based on their personal or family medical history. Genetic testing can help identify specific gene mutations, such as BRCA1 and BRCA2, which increase the risk of developing breast cancer.
If any abnormality is detected through screening or if you notice any changes in your breasts, it is essential to follow up with your healthcare provider for further evaluation and appropriate diagnostic tests. Early detection through regular screenings and timely follow-up can significantly improve the chances of successful treatment and positive outcomes in breast cancer cases.
Stages of Breast Cancer
Breast cancer staging is a critical process that helps healthcare professionals determine the extent and progression of the disease. Staging provides valuable information for developing an appropriate treatment plan and predicting the prognosis. The stages of breast cancer are classified based on the size of the tumor, lymph node involvement, and whether the cancer has spread to other parts of the body. Here’s an overview of the stages of breast cancer:
- Stage 0: Stage 0, also known as carcinoma in situ, refers to non-invasive breast cancer. It is characterized by abnormal cells that are confined to the milk ducts (ductal carcinoma in situ, or DCIS) or lobules (lobular carcinoma in situ, or LCIS). At this stage, the cancer has not spread to nearby tissues or lymph nodes.
- Stage I: Stage I breast cancer is divided into two subcategories: IA and IB.
- Stage IA: The tumor is small, measuring up to 2 centimeters, and has not spread to the lymph nodes or other areas of the body.
- Stage IB: There is either no tumor in the breast, but small clusters of cancer cells are found in the lymph nodes, or the tumor measures up to 2 centimeters and has spread to nearby lymph nodes.
- Stage II: Stage II breast cancer is also divided into two subcategories: IIA and IIB.
- Stage IIA: This stage includes one of the following conditions:
- The tumor measures up to 2 centimeters and has spread to 1-3 axillary (underarm) lymph nodes.
- The tumor measures between 2-5 centimeters but has not spread to the lymph nodes.
- Stage IIB: This stage includes one of the following conditions:
- The tumor measures between 2-5 centimeters and has spread to 1-3 axillary lymph nodes.
- The tumor measures larger than 5 centimeters but has not spread to the lymph nodes.
- Stage IIA: This stage includes one of the following conditions:
- Stage III: Stage III breast cancer is divided into three subcategories: IIIA, IIIB, and IIIC.
- Stage IIIA: This stage includes one of the following conditions:
- The tumor measures up to 5 centimeters, and cancer has spread to 4-9 axillary lymph nodes.
- The tumor is larger than 5 centimeters, and cancer has spread to 1-3 axillary lymph nodes.
- The tumor is larger than 5 centimeters, and cancer has spread to internal mammary lymph nodes.
- Stage IIIB: In this stage, the cancer may have spread to the chest wall or the skin of the breast. It may also cause swelling or ulceration of the breast or may involve 9 or more axillary lymph nodes.
- Stage IIIC: This stage includes one of the following conditions:
- The cancer has spread to 10 or more axillary lymph nodes.
- The cancer has spread to the lymph nodes above or below the collarbone.
- The cancer has spread to the internal mammary lymph nodes and axillary lymph nodes.
- Stage IIIA: This stage includes one of the following conditions:
- Stage IV: Stage IV, also known as metastatic breast cancer, indicates that the cancer has spread to other parts of the body, such as the bones, liver, lungs, or brain. At this stage, treatment focuses on managing the disease and improving the quality of life.
Breast cancer staging provides crucial information for determining the most appropriate treatment approach. It helps healthcare professionals tailor treatment plans to the specific characteristics of the cancer and its stage. Regular screenings and early detection play a significant role in identifying breast cancer at earlier stages when treatment options are generally more effective.
Treatment Options for Breast Cancer
The treatment of breast cancer depends on various factors, including the stage of the cancer, the characteristics of the tumor, and the individual’s overall health. A multidisciplinary approach involving a team of healthcare professionals is often employed to develop a comprehensive treatment plan. Here are the common treatment options for breast cancer:
Surgery
Surgery is a primary treatment option for breast cancer and involves removing the cancerous tumor and surrounding tissue. The types of surgical procedures include:
Lumpectomy
Also known as breast-conserving surgery, this procedure removes the tumor and a small margin of healthy tissue around it, preserving the rest of the breast.
Mastectomy
In this procedure, the entire breast is removed. Depending on the extent of the cancer and individual circumstances, a simple mastectomy or a modified radical mastectomy (which also involves removing the axillary lymph nodes) may be performed.
Breast Reconstruction
Reconstruction surgery can be performed at the time of the mastectomy or at a later stage to rebuild the breast’s shape and appearance.
Radiation Therapy
Radiation therapy uses high-energy X-rays or other forms of radiation to kill cancer cells and reduce the risk of cancer recurrence. It is commonly used after breast-conserving surgery or mastectomy to target any remaining cancer cells in the breast, chest wall, or nearby lymph nodes.
Chemotherapy
Chemotherapy involves the use of powerful drugs to destroy cancer cells throughout the body. It can be administered intravenously or in pill form, and it is typically used to treat breast cancer that has a higher risk of spreading or has already spread to other parts of the body. Chemotherapy may be given before surgery (neoadjuvant) to shrink tumors, after surgery (adjuvant) to eliminate any remaining cancer cells, or in advanced cases to manage the disease.
Hormone Therapy
Hormone therapy is primarily used to treat hormone receptor-positive breast cancers, where the cancer cells have receptors for estrogen or progesterone. This treatment aims to block the effects of hormones on cancer cells or reduce hormone production in the body. It can be administered through medications such as selective estrogen receptor modulators (SERMs), aromatase inhibitors, or ovarian suppression.
Targeted Therapy
Targeted therapy drugs specifically target certain characteristics of cancer cells that promote their growth and survival. One common type of targeted therapy for breast cancer is HER2-targeted therapy, which is used for HER2-positive breast cancers. These drugs can help block the HER2 protein and slow down or eliminate cancer cell growth.
Immunotherapy
Immunotherapy is an innovative treatment approach that stimulates the body’s immune system to recognize and attack cancer cells. While still being researched for breast cancer treatment, immunotherapy has shown promising results, particularly for certain subtypes of breast cancer.
Clinical Trials
Participation in clinical trials provides access to innovative treatment options and helps advance the field of breast cancer research. Clinical trials evaluate new drugs, treatment approaches, and therapies to improve outcomes and provide better treatment options for breast cancer patients.
The choice of treatment depends on various factors, including the stage and characteristics of the cancer, the individual’s overall health, and personal preferences. Treatment plans are often tailored to meet the unique needs of each patient. It is important to have open and honest discussions with healthcare professionals to understand the available treatment options, potential side effects, and expected outcomes.
Breast cancer treatment is often multimodal, combining different approaches to achieve the best results. The goal is to remove or control the cancer while preserving or restoring quality of life. With advancements in medical technology and ongoing research, treatment options for breast cancer continue to evolve, offering improved outcomes and a better prognosis for those affected by this disease.
Supportive Care for Breast Cancer Patients

Dealing with breast cancer can be an incredibly challenging and overwhelming experience, not only physically but also emotionally. That’s why it is crucial to have access to a comprehensive support system that can provide guidance, understanding, and encouragement throughout the journey. In addition to medical treatments, supportive care plays a vital role in improving the well-being and quality of life for breast cancer patients. One such remarkable organization is GD Caring and Sharing Cancer Support Group, which is dedicated to supporting, motivating, and inspiring those affected by cancer.
GD Caring and Sharing Cancer Support Group understands the unique needs of individuals facing a breast cancer diagnosis. Their mission is to provide a nurturing and compassionate environment where members can find solace, strength, and valuable resources to navigate the challenges of cancer. Here are some ways in which supportive care can help breast cancer patients:
- Emotional Support: Dealing with a cancer diagnosis can evoke a wide range of emotions, including fear, anxiety, sadness, and uncertainty. Support groups like GD Caring and Sharing Cancer Support Group provide a safe space for individuals to express their feelings, share experiences, and receive empathy from others who truly understand what they are going through. The emotional support received from peers and trained facilitators can be invaluable in promoting mental well-being and resilience.
- Information and Education: Understanding the intricacies of breast cancer, treatment options, and potential side effects can empower patients to make informed decisions about their care. Supportive care groups often offer educational resources, workshops, and expert presentations to provide accurate and up-to-date information. This knowledge equips patients with the tools necessary to actively participate in their treatment plans and communicate effectively with their healthcare team.
- Coping Strategies: Support groups can provide practical guidance on coping with the physical and emotional challenges of breast cancer. Members can share strategies for managing treatment side effects, reducing stress, improving sleep, and maintaining a healthy lifestyle. Learning from others who have faced similar situations can offer valuable insights and practical tips that can enhance the overall well-being of patients.
- Peer Connection: Connecting with individuals who have gone through or are currently going through similar experiences can provide a sense of belonging and validation. Supportive care groups foster peer connections, allowing breast cancer patients to build relationships, offer mutual support, and form lasting friendships. Sharing stories, milestones, and triumphs with fellow group members can instill hope and inspire one another to persevere through the challenges.
- Practical Support: In addition to emotional and informational support, supportive care organizations like GD Caring and Sharing Cancer Support Group may offer practical assistance to breast cancer patients. This can include providing access to financial resources, transportation services, wigs or head coverings, assistance with daily activities, and referrals to community resources for additional support.
Navigating the complexities of breast cancer requires a comprehensive approach that addresses both the physical and emotional aspects of the disease. Supportive care, offered by organizations like GD Caring and Sharing Cancer Support Group, plays a vital role in empowering breast cancer patients and their families to face the challenges with strength, resilience, and a sense of community. By providing the necessary tools, resources, and a caring environment, supportive care groups aim to enhance the overall well-being and quality of life for those affected by breast cancer.
Breast Cancer Prevention
Breast cancer prevention involves taking proactive steps to reduce the risk of developing this disease. While some risk factors, such as age and family history, cannot be controlled, there are lifestyle choices and strategies that can help lower the likelihood of developing breast cancer. By adopting a healthy lifestyle and staying informed about risk factors, individuals can empower themselves to make choices that may reduce their risk. Here are some key measures for breast cancer prevention:
- Regular Breast Self-Exams: Performing regular breast self-exams is an important step in detecting any changes or abnormalities in the breasts. By becoming familiar with the normal look and feel of their breasts, individuals can identify potential warning signs, such as lumps or changes in size or texture. If any unusual changes are noticed, it is important to consult a healthcare professional for further evaluation.
- Clinical Breast Exams: Regular clinical breast exams by a healthcare professional are recommended to detect any potential abnormalities. These exams involve a thorough examination of the breasts and surrounding areas to identify any signs or symptoms that may require further investigation. Clinical breast exams can complement self-exams and provide an additional layer of vigilance in monitoring breast health.
- Mammograms: Mammograms are specialized X-ray examinations that can detect breast cancer in its early stages, even before any symptoms are present. Regular screening mammograms are recommended for women based on age and individual risk factors. These screenings can help identify breast cancer at its earliest and most treatable stages, increasing the chances of successful treatment and positive outcomes.
- Lifestyle Choices: Adopting a healthy lifestyle can significantly contribute to breast cancer prevention. Here are some lifestyle choices that may reduce the risk:
- Maintain a Healthy Weight: Being overweight or obese increases the risk of developing breast cancer, particularly after menopause. Engaging in regular physical activity and following a balanced diet can help maintain a healthy weight.
- Limit Alcohol Consumption: Excessive alcohol consumption has been linked to an increased risk of breast cancer. It is advisable to limit alcohol intake or avoid it altogether.
- Quit Smoking: Smoking has been associated with an increased risk of breast cancer, along with numerous other health problems. Quitting smoking and avoiding exposure to secondhand smoke can have multiple health benefits.
- Balanced Diet: Eating a nutritious diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can support overall health and potentially reduce the risk of breast cancer.
- Hormone Replacement Therapy: If considering hormone replacement therapy for menopausal symptoms, it is important to discuss the potential risks and benefits with a healthcare professional. Prolonged use of hormone replacement therapy may increase the risk of breast cancer.
- Know Your Risk Factors: Understanding your personal risk factors for breast cancer can help guide preventive measures. Some risk factors, such as family history and genetic mutations like BRCA1 and BRCA2, cannot be changed. However, knowing about these factors can prompt more vigilant screening and monitoring. Discussing individual risk factors with a healthcare professional can provide personalized recommendations for prevention and early detection.
Remember, while these preventive measures can reduce the risk of breast cancer, they do not guarantee complete prevention. Regular screenings, self-exams, and maintaining open communication with healthcare professionals remain essential components of breast health. By being proactive and making informed choices, individuals can take important steps towards reducing the risk of breast cancer and promoting overall well-being.
The Conclusion
Breast cancer is a complex and challenging disease that affects millions of individuals worldwide. Throughout this comprehensive guide, we have explored various aspects of breast cancer, including its introduction, types, risk factors, symptoms, screening and diagnosis, stages, treatment options, supportive care, prevention, and more. By understanding these crucial aspects, we hope to have empowered you with knowledge and awareness to make informed decisions regarding your breast health.
Early detection remains a key factor in improving breast cancer outcomes. Regular breast self-exams, clinical breast exams, and mammograms can help identify any abnormalities or warning signs at an early stage when treatment options are most effective. It is important to stay vigilant, know your own body, and promptly report any changes to your healthcare provider.
Furthermore, we have highlighted the importance of a multidisciplinary approach to breast cancer treatment, involving surgery, radiation therapy, chemotherapy, hormone therapy, targeted therapy, immunotherapy, and participation in clinical trials. Each treatment option is tailored to individual circumstances, and discussions with healthcare professionals can guide the most suitable treatment plan.
We have also emphasized the significance of supportive care throughout the breast cancer journey. Organizations like GD Caring and Sharing Cancer Support Group provide invaluable emotional support, information, coping strategies, and practical assistance to individuals affected by breast cancer. Connecting with peers who have shared experiences can provide comfort, inspiration, and a sense of community during challenging times.
Breast cancer prevention plays a vital role in reducing the risk of developing this disease. By maintaining a healthy lifestyle, performing regular self-exams, undergoing clinical exams and mammograms, and understanding personal risk factors, individuals can take proactive steps towards minimizing their risk. Remember, prevention is a combination of self-care, informed choices, and staying informed about advancements in breast cancer research and screening technologies.
In conclusion, breast cancer is a formidable adversary, but with early detection, effective treatments, supportive care, and a commitment to prevention, it is a battle that can be fought and won. Stay proactive, prioritize your breast health, and lean on the support systems available to you. Together, we can continue to raise awareness, promote early detection, and improve the lives of those affected by breast cancer.
Remember, you are not alone in this journey. Reach out to healthcare professionals, support groups, and loved ones who can provide the guidance, care, and encouragement needed to face breast cancer with strength and resilience. Stay informed, stay empowered, and stay committed to your well-being.
With determination, compassion, and ongoing research, we can create a future where breast cancer is no longer a threat to the lives of our loved ones. Let us stand together in the fight against breast cancer and strive for a world free from its grasp.
